We knew. We have been warned about emerging infectious diseases over, and over, and over for years. And we did nothing, or close to it. Our political leaders have failed us, we as citizens have failed ourselves by not holding them accountable, and the only thing one could reliably predict based on what we have learned over the last two years is that when — not if but when — the next pandemic comes, “they” are not coming to help.
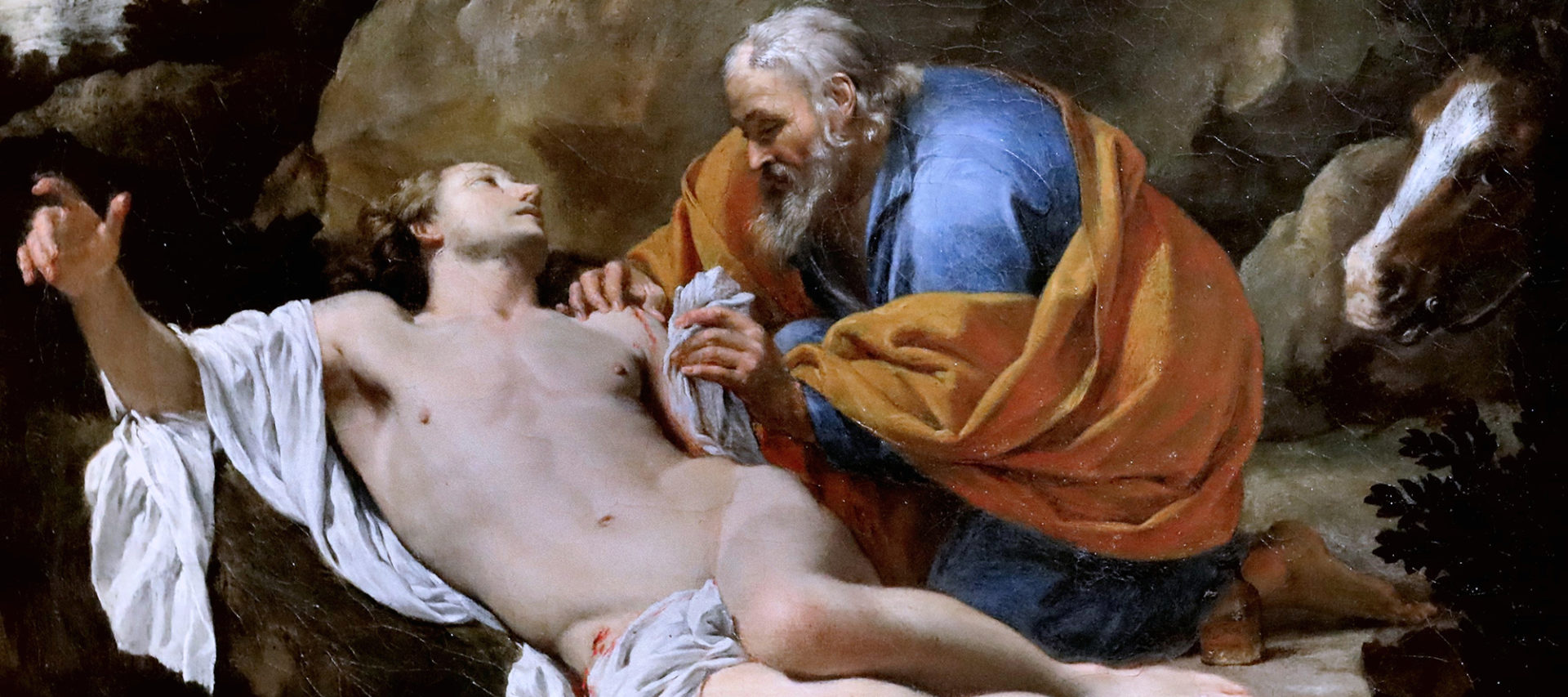
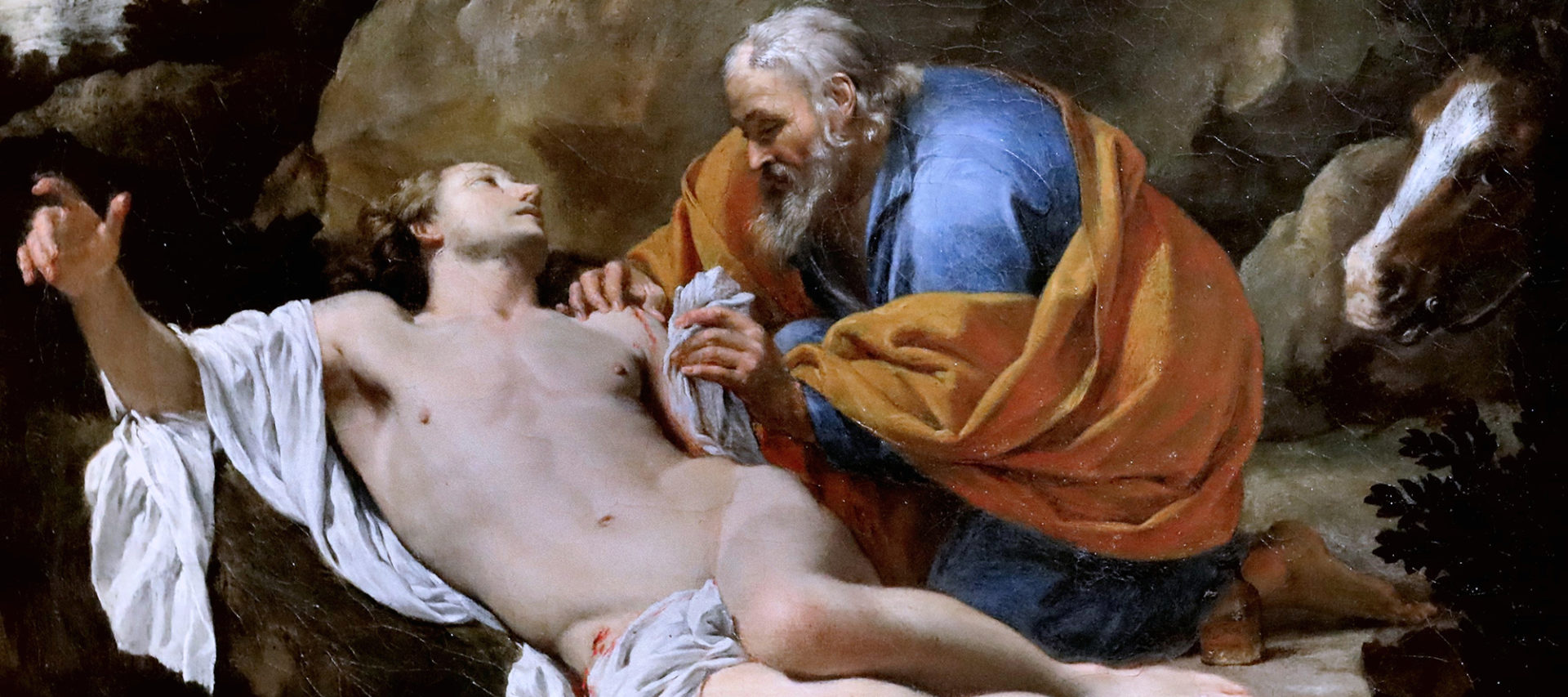
But let’s not respond to madness with depression or apathy. There is a lot we could do, and a popular movement can help to get it done — groups of people that Pope Francis has called “social poets” and “collective Samaritans.” Here is a policy agenda for anyone of goodwill to use in service of the common good, dedicated to the popular movement in the United States. You are eagerly awaited.
Let’s begin with the animals. “The first thing to understand is that whatever future threats we’re going to face already exist; they are currently circulating in wildlife. Think of it as viral dark matter.” Thus said Dennis Carroll, the former head of the U.S. Agency for International Development’s project on spillover viruses. Diseases spilling over from animals to humans typically kill 2.7 million people each year, with most of these deaths concentrated among the world’s poorest. As much of creation migrates in response to climate change, and humanity continues to encroach on once wild habitats, animal viruses will spill over to humans more often.
In theory, we could go on the offensive in this fight. We already have tools to monitor animal migration patterns, collect samples, catalog viruses, and analyze their relative spillover risk. We just don’t spend enough money using these tools effectively. Even in 2021, a year into the Covid-19 pandemic, the United States spent just $670 million on global health security, barely more than the Pentagon spent training “moderate Syrian rebels,” if anyone remembers those.
We will also need to get a lot better at making vaccines against these diseases. Given the news stories of recent years, you would think that we make new vaccines all the time. But we make almost none. There are hundreds of diseases we could develop vaccines against today but don’t — not because the science isn’t there, but because they are bad business in the absence of a crisis that spurs governments to invest. Writing in May 2020 for the Drug Information Association’s Global Forum, a group of researchers argued that private pharmaceutical companies lack the financial incentive to invest in vaccine R&D, making them dependent on government investment. Looking back at America’s Covid vaccine development now, we can see that it has been a scientific and financial success in large part because the government has for years been laying the groundwork of vaccine investment, allowing for quick targeting of resources in 2020.
Going forward, the public sector has to step up, which means not just the U.S. government but us. One promising idea is to create a public fund in the style found in many countries around the world, and in Alaska, to steward a common resource for the common good when private sector incentive is lacking. Matt Bruenig’s proposal of a Social Wealth Fund may be a guide. With the help of such a fund, it should not be difficult to invest the $35 billion that the Global Forum authors say are needed to finance the creation of the 141 vaccines targeting the most deadly pathogens identified by the Coalition for Epidemic Preparedness Innovations.
The United States government, however geriatric and sclerotic it has become, can still throw a punch when it needs to — and in this case it will. But increased public-sector involvement in vaccine development need not rely only on vast government spending. Other public funding is possible, and it should not stop with vaccine development but should extend also to vaccine manufacturing and distribution.
We must also reform the clinical trial process for vaccines. The speed of development of the Covid vaccines should be a model going forward, one we can further improve. We can have all the funding in the world and still succumb to future pandemics if we don’t figure out how to speed up the long development timeline for most vaccines.
The Pfizer vaccine was designed in just a few hours. It then took nearly a year to get to the public. A lot of people died over that year, and the Pfizer vaccine was about as safe as vaccines typically are. Russia’s SputnikV vaccine was authorized in half the time it took the FDA to authorize Pfizer, even though the Russian approval was based on data from early trials with just seventy-six participants. Russia’s decision was excoriated as reckless, but it turned out that the two vaccines were quite similar in safety and efficacy. It’s hard not to conclude that we have probably accepted hundreds of thousands of Covid deaths while taking time to perform costly tests to identify health risks like blood clots and allergic reactions that, while important, affect only a very small fraction of those who take vaccines. Given the vigorous debates we did have, it was a shame we didn’t have this one — that there were vaccines available that could have saved lives immediately.
To get more aggressive on trials we should consider three things. First, we should create a Civilian Vaccine Corps — a volunteer base of people committed to serving as large-scale trial participants. Finding and recruiting participants for a large medical trial is a huge project, and we need a reserve of volunteers to help. Such an initiative should earn compensation as well as the kind of honor conferred from serving in the Peace Corps or as a volunteer firefighter. Second, we should open our protocols up to the possibility of human challenge trials. Over 38,000 young people volunteered to be exposed to Covid-19 to help accelerate the speed of testing and approving new vaccines. This is a remarkable act of charity. We should have the ability to conduct such trials safely and efficiently with informed volunteers. Third, we should consider whether or not to license both a “full” vaccine and a “rapid” version, just as we do with Covid-19 test kits.
Finally, we must touch on supply chain and manufacturing issues. We desperately need to re-shore and decentralize our personal protective equipment and medical supply chains. The RadVac experiment in open-source vaccines designed with decentralized production in mind is a very encouraging model that should be tested immediately. The logistical challenge of shipping vaccines on dry-ice storage over large distances drives up the price of distribution, and it also makes the supply chain more vulnerable than one built around local production.
The United States has about 30 percent of the manufacturing facilities and resources needed to make enough active pharmaceutical ingredients, the core components of generic drugs, to supply the U.S. market. And we still have little capability for making masks, gowns, medical gloves, and other supplies domestically. We must never again let our doctors need to duct-tape their own masks together or send grandparents to the grocery store with a flimsy paper mask to protect them. Legislation like the American PPE Supply Chain Integrity Act is the sort of bold response we need to address this challenge.
All this is just a start. As David Sencer wrote in 1971, when he was director of the CDC: “And so infectious disease, one of man’s oldest enemies, survives as an adversary that calls forth our best efforts.” But at the same time we must bear in mind Pope Francis’s warning in 2020: “Radical individualism is a virus that is extremely difficult to eliminate, for it is clever.” This is why to combat infectious disease we need more than science and money; we need solidarity. Again Pope Francis:
Solidarity means much more than engaging in sporadic acts of generosity. It means thinking and acting in terms of community. It means that the lives of all are prior to the appropriation of goods by a few…. Solidarity, understood in its most profound meaning, is a way of making history, and this is what popular movements are doing.
Exhausted by science and tech debates that go nowhere?